Key word:CKD (Chronic Kidney Disease)
Chronic Kidney Disease (CKD) and L-FABP
L-FABP level in urine is correlated with the degree of tubulointerstitial injury in human kidney tissue[1]. This biomarker reflects stress which is loaded on the renal tubule and some clinical studies on non-diabetic chronic kidney disease patients have determined its utility in the prediction of renal prognosis[2]. Urinary L-FABP is more sensitive than urinary protein in predicting the progression of CKD. Also, urinary L-FABP level increases and decreases respectively according to the progression and relief of kidney disease. Therefore, this biomarker is useful for its monitoring.
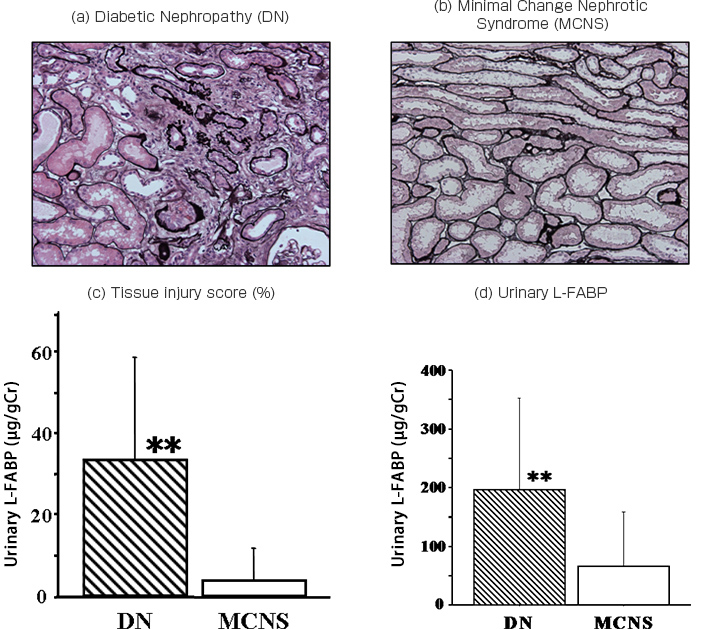
A-1: Comparison of histological renal tubulointerstitial damage and creatinine corrected urinary L-FABP level between Diabetic Nephropathy (DN) and Minimal Change Nephrotic Syndrome (MCNS)
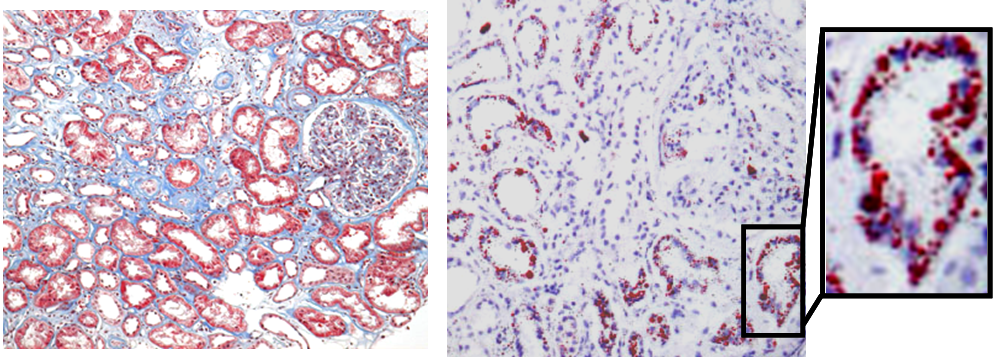
A-2: Histological evaluation of tubulointerstitial damage (Masson’s Trichrome stain and Suda III stain)
In diabetic nephropathy, stronger tubulointerstitial injury compared to MCNS was found, and adipose accumulation in renal tubules was confirmed.
(e) Diabetic Nephropathy (DN)
Masson’s Trichrome stain (left) and Sudan III stain(right)
(f) Minimal Change Nephrotic Syndrome (MCS)
Masson’s Trichrome stain (left) and Sudan III stain(right)
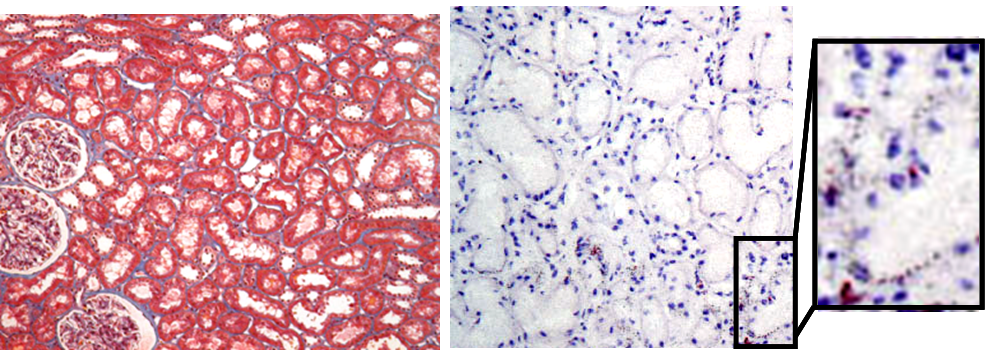
(Partly modified from figure 1 and figure 2 of article [3])
FIGS. a,b e,f
Pathological tissue images (x100) of (a) Diabetic Nephropathy (DN) and (b) Minimal Change Nephrotic Syndrome (MCNS).
FIGS. c,d
(c) Tubulointerstitial injury score (%) for both disease groups and (d) urinary L-FABP (mean ± standard deviation, **p<0.01 vs. MCNS)(No significant differences seen in other urinary markers in both disease groups)
Subjects
8 cases presenting nephrosis syndrome diagnosed as diabetic nephropathy by renal biopsy and 12 cases with MCNS were examined to determine the correlation between histological tubulointerstitial lesion and urinary biomarker level in CKD patients.
Method
Urine was collected from the above subjects during 24 hours from hospital admission. Urinary protein, albumin, NAG and L-FABP levels and histopathological analysis results were compared for both groups.
Results
No significant difference was found in both groups in protein, albumin and NAG level in urine but significantly high concentration were shown in urinary L-FABP only in the diabetic nephropathy cases. These results correspond with these of histological tubulointerstitial injury evaluations (FIGS. c, d).
The conventional urinary biomarkers were not able to differentiate the degree of severity of tubulointerstitial injury in nephrotic syndrome patients however only urinary L-FABP level was determined. This result suggests that urinary L-FABP level may reflect specifically tubular injury in early stage diabetic nephropathy patients.
B: Comparison of L-FABP levels in blood and urine (kidney disease specificity of urinary L-FABP)
Comparison of (a) blood L-FABP and (b) urinary L-FABP in liver disease patients (71 cases ), CKD patients (73 cases
), CKD patients (73 cases ), and healthy subjects (71 cases
), and healthy subjects (71 cases )
)
(Mean ± standard deviation,  *p<0.05 vs. healthy subjects,
*p<0.05 vs. healthy subjects,  $p<0.05 vs. CKD patients,
$p<0.05 vs. CKD patients,  #p<0.05 vs. liver disease patients )
#p<0.05 vs. liver disease patients )
(Partly modified from figure 3 of article [4])
Subjects
L-FABP is also expressed in the liver and intestinal tract hence the possibility of blood L-FABP level increase in the cases of liver or intestinal diseases would be conceived. Some clinical research centers are thinking about the new study whether urinary L-FABP level would be affected by blood L-FABP level.
The results of blood and urinary L-FABP measurements for 71 liver disease patients with normal kidney function ( ), 73 CKD patients with normal liver function (
), 73 CKD patients with normal liver function ( ), and 71 healthy subjects (
), and 71 healthy subjects ( ) are shown above.
) are shown above.
In liver disease patients with normal kidney function, their blood L-FABP level was significantly high which was more than 7 times greater than that of healthy subjects, but it there is no significant difference in urinary L-FABP level compared with healthy subjects.
Meanwhile, in CKD patients with normal liver function, their urinary L-FABP level was significantly high compared to both healthy subjects and liver disease patients and their blood L-FABP level tends, not significantly but, to increase compared with healthy subjects. This is thought to be caused by a clearance decrease in CKD patients.
Results
The past investigations deduct that even if the diseases show high blood L-FABP level but with normal kidney function, L-FABP level in urine is not affected. This is not influence due to gender and age.
Urinary L-FABP is thought to be renal disease specific indicator which reflect sensitively tubular disorder in a different way than the conventional urinary biomarker such as NAG and α1M and to be excreted into the urine by kidney tissue.
References
- [1] Kamijo, A. et al., Urinary excretion of fatty acid-binding protein reflects stress overload on the proximal tubules. Am J Pathol. 165(4): 1243-1255, 2004. PubMed
- [2] Kamijo, A. et al., Clinical evaluation of urinary excretion of liver-type fatty acid-binding protein as a marker for the monitoring of chronic kidney disease: A multicenter trial. J Lab Clin Med. 145(3): 125-133, 2005. PubMed
- [3] Sasaki, H. et al., Urinary fatty acids and liver-type fatty acid binding protein in diabetic nephropathy. Nephron Clin Pract. 112(3): c148-156, 2009. PubMed
- [4] Kamijo, A. et al., Urinary liver-type fatty acid binding protein as a useful biomarker in chronic kidney disease. Mol Cell Biochem. 284(1-2): 175-182, 2006. PubMed